Covid-19: Black and brown Americans brace for the worst

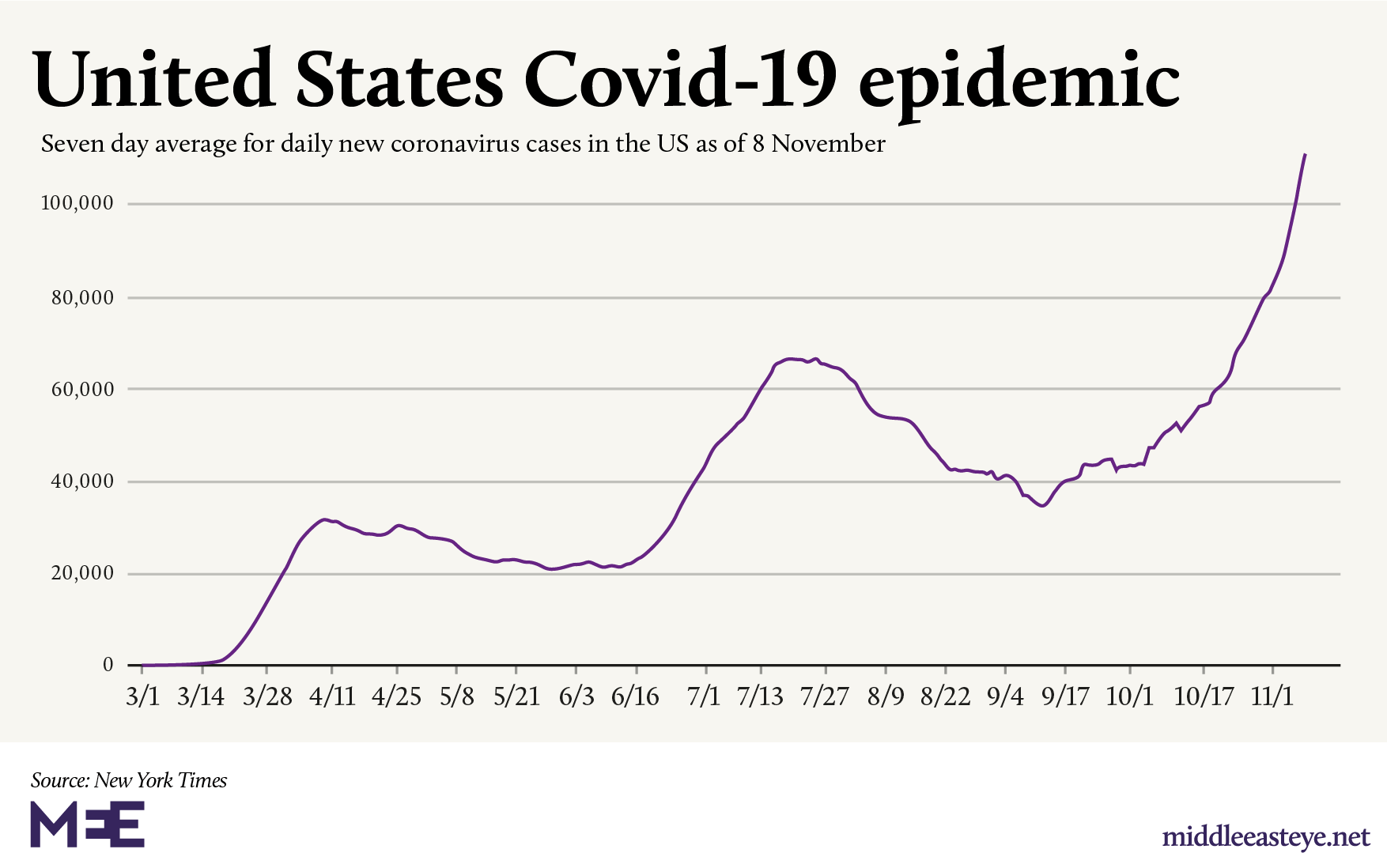
A rudderless president, a flailing economy and continued political uncertainty mean that a second wave of the coronavirus is now taking root in the United States - and could be more disastrous than the first.
Across the country, doctors are raising the alarm and pleading with Americans to follow social distancing measures and wear masks, as hospitals begin to fill up and death rates start to slide out of control once again.
Around 1,000 people have died every day since the start of November.
Over the past week alone, the New York Times noted, "there has been an average of 150,265 cases per day, an increase of 81 percent from the average two weeks earlier".
There are more people in hospital now than any other point in the pandemic. Numbers are well beyond the spring peak of 59,940, on 15 April, and the summer peak of 59,718 on 23 July.
New MEE newsletter: Jerusalem Dispatch
Sign up to get the latest insights and analysis on Israel-Palestine, alongside Turkey Unpacked and other MEE newsletters
But health experts say that behind the statistics lies another morbid fact.
As the virus spreads and deepens, it will be working class people, particularly Black and brown people, who will be hit the hardest.
The first wave of the Covid-19 devastated working class communities in New York City. Facing job cuts, millions had to confront housing and food insecurity. The pandemic pulverised community action, including the setting up of mutual aid groups and food pantries.
But with business yet to recover and jobs still to return, exhaustion has set in and efforts are waning. Experts say a repeat of the epidemic in the spring could be devastating.
Black people bearing the brunt
Since the pandemic reached American shores, there have been 11 million confirmed Covid-19 cases with more than 244,207 deaths.
But unlike the first wave that peaked in April and May, the virus is no longer concentrated in one or two states.
Large swathes of the US, from Wyoming and Iowa to North and South Dakota, have seen Covid-19 infections skyrocketing.
According to the Covid Tracking Project, 27 states have hit new highs for the number of cases reported. In some of these states, Black people continue to bear the brunt.
In Michigan, where Black people make up 14 percent of the population, they make up an estimated 34 percent of all Covid-19 deaths.
In the District of Columbia, where Black people make up 32 percent of the population, they make up an estimated 45 percent of Covid-19 related deaths.
In New York state, Black people make up 32 percent of all Covid deaths despite comprising just 14 percent of the population.
'We need to get support to the most vulnerable Americans immediately, especially the Black and Brown communities in my district [that] have been some of the hardest hit by the pandemic'
- Congresswoman Ilhan Omar
The numbers reiterate findings of a study published last week by the Lancet that people of Black and Asian descent were not only at a greater risk of contracting the virus, but that Asians faced a higher risk of being admitted into hospital or dying than whites because of the socio-economic factors faced by the demographic.
"Our findings suggest that the disproportionate impact of Covid-19 on Black and Asian communities is mainly attributable to increased risk of infection in these communities," Manish Pareek, the paper's senior author and an associate clinical professor in infectious diseases at the University of Leicester, said in a statement.
"It is shameful that this Administration and their Senate counterparts continue to ignore people's basic needs," Congresswoman Ilhan Omar told Middle East Eye.
"We need to get support to the most vulnerable Americans immediately, especially the Black and Brown communities in my district [that] have been some of the hardest hit by the pandemic, yet are the least likely have their needs met."
Not only are people of colour more likely to be doing essential jobs, they are also most likely to be taking public transport or returning to cramped housing.
The same demographic is more likely to have poor health insurance, have underlying health problems such as obesity and hypertension, and face discrimination at hospitals.
"For someone who lives paycheque to paycheque, who doesn’t have money next week, is not working an option for them? No, it's not, and these folks will get sick," Aamnah Khan, an activist with Desis Rising Up and Moving (Drum), said.
"If the most vulnerable are not safe, then no one is."
Delay in receiving test results
Research also indicates that people of colour can wait almost a day longer than white people to receive test results.
A separate analysis by the Kaiser Family Foundation found that nursing homes with larger populations of Black or Hispanic residents suffered more Covid-19 infections and deaths. This underlines the fact that although white Americans make up the most number of deaths in absolute terms, Black people and people of colour were impacted most.
Compounding the collection of data is the fact that not all states collect race data when it comes to the virus.
"The clearest statement we can make at the national level is that Black people account for 20 percent of US Covid-19 deaths where race is known," Erin Kissane, the managing editor of the Covid Tracking Project, told Middle East Eye.
Black people make up 13 percent of the overall population.
"We don't yet know how the current surge of infections will play out demographically, but each weekly update we do includes a short update about what we're learning as the surge moves from low-population states with overwhelmingly white populations to high-population states that are more racially and ethnically diverse," Kissane added.
A report from the Centre for Disease Control (CDC) released on Friday showed that a majority of those hospitalised for the virus continue to be Black or Hispanic.
Data from the report showed that the hospitalisation rate among the Hispanic or Latino population, Native Americans and Black population was close to four times that of white Americans.
'The second wave is here'
With little direction from the White House and the national media fixated on an unprecedented political crisis unfolding over President Donald Trump's refusal to concede, those on the front lines in hospitals are growing increasingly frustrated.
Up to 14 states have yet to issue a mandate to wear masks in public.
Uneven and inconsistent policies across states, often meaningless lockdown plans and the continued politicisation of basics such as wearing masks, have left health workers weary.
CNN reported last week that staffing levels were so dire in some hospitals that asymptomatic doctors and nurses infected with coronavirus are allowed to keep working in Covid-19 units. Health workers were watching their colleagues fall ill and were "worn out and tired and scared", one doctor was quoted as having said.
Meanwhile, hospitals are starting to heave as patients begin to flood emergency rooms. This week, nurses in Pennsylvania embarked on a strike over what they called unsafe working conditions.
"Three weeks ago, we were dealing with six or seven patients whom we would discover had Covid-19," Syed Hassan, an doctor working in internal medicine at a hospital in New Jersey, told MEE.
"Now we are seeing around 50 a day, arriving and displaying Covid-19 symptoms. We are resigned to the fact that the second wave is here.
"And the way it's going, it's simply too early to know how bad it's going to be."
In neighbouring New York City, the centre of much of the first wave, where by May one in 500 residents had died from the virus, doctors working in boroughs such as Queens and the Bronx told MEE that they were preparing for the worst.
"Personally, I was seeing maybe seven patients in a 24-hour period. Last week it jumped to 42 patients. These are people who are suffering from hypoxia or other Covid-19 symptoms," Nauman Piracha, a doctor in NYC, told MEE.
'Covid fatigue'
Over the weekend, New York Governor Andrew Cuomo appeared to acknowledge what he described as "Covid fatigue", as the pandemic moves into its ninth month. But he urged New Yorkers to adhere to gathering limits and the oncoming surge.
"What we're seeing now as Covid rages across the country and world is what scientists told us time and time again would happen as the colder months arrived," Cuomo said.
Though the numbers are rising in hospitals, and the Covid Tracking Project say the "dangerous spike in hospitalizations suggests that further increases in the number of fatalities are imminent," doctors in NYC told MEE that doctors were are experiencing a little more success on the treatment front.
'Where did we get the trillions of dollars to bail out companies? We really need these things in place so that volunteers trying to help people don't have to risk their lives'
- Aamnah Khan, Drum
"We are seeing a rise in patients but the death toll is not as high as earlier in the year," Piracha, the NYC doctor, told MEE.
Though doctors suspect that earlier interventions, a better understanding of the cocktail of treatment required and a lighter strain of the virus may be some of the reasons fatalities are lower, few health professionals are likely to suggest having a better grasp of the virus.
"We are seeing fewer deaths, but people are still getting really sick and if they recover they still have after-effects to deal with. These can be horrific," a doctor from the Bronx, said. "We are asking people to please adhere to social distancing and to wear masks."
But even with the rising optimism over better treatment and the possibility of a vaccine, researchers say that authorities have still to prioritise minimising exposure to high-risk communities and to dedicating more resources to tackle the disparities that are leading to more infections and deaths.
Others, like Lawrence Gostin, a professor of global health law at Georgetown University, are calling for a future vaccine to be prioritised for people of colour.
"The reason is both because of historic structural racism that’s resulted in grossly unequal health outcomes for all kinds of diseases and because Covid-19 has so disproportionately impacted the lives of people of colour," Gostin said.
'Grim situation'
But in a country still divided over whether people ought to wear masks or adhere to social-distancing measures, there is little expectation that systemic issues will be addressed anytime soon.
Though the unemployment rate has reduced since the early days of the pandemic, millions are still jobless, facing eviction and homelessness. Where small businesses are teetering on the verge of bankruptcy, lawmakers have yet to agree on a second stimulus package to bail out the poor.
"I'm seeing a lack of leadership, not just from the president, but from our mayor and governor in addressing these things. If the governor wanted to, he could freeze rent right now but he refuses to. If he wanted, he could create separate funding for those not covered," Khan, from Drum, said.
"Where did we get the trillions of dollars to bail out companies? We really need these things in place so that volunteers trying to help people don’t have to risk their lives. But for the time being, we are still doing that work of building out mutual aid work and connections," Khan added.
Meanwhile, the death march continues.
The current national case surge, the Covid Tracking Project notes, has been underway for nine weeks; hospitalisations have risen for seven weeks and deaths have risen for five. In the 16-page Minnesota section of the Star Tribune newspaper on 15 November, one Twitter user noted that 10 of the pages were taken up with obituaries.
Kissane, the managing editor of the Covid Tracking Project, said that one of the difficulties with covering the pandemic is that the nature of the virus meant there was often a lag between the rise in hospitalisations and fatalities.
"I can say that with these case and hospitalisation numbers, the patterns we've seen so far in the pandemic would suggest that deaths will rise and stay high until a few weeks after the current case surge is brought under control, but I can't speculate about totals.
"The lag in death reporting makes the severity of the pandemic difficult to cover as a surge is accelerating - we know a lot of people are dying today in American hospitals, we won't see them show up in the data for another three weeks.
"So cases rise and there's a delay and then hospitalisations rise and there's a delay and then by the time deaths spike, we are probably already locked into a very grim situation."
Middle East Eye delivers independent and unrivalled coverage and analysis of the Middle East, North Africa and beyond. To learn more about republishing this content and the associated fees, please fill out this form. More about MEE can be found here.



![BLM New Jersey [Azad Essa/MEE]](/sites/default/files/NJ%20BLM5.jpg)
![BLM New Jersey [Azad Essa/MEE]](/sites/default/files/NJ%20BLM4.jpg)


